You might be facing involuntary muscle contractions, odd twisting postures, or repetitive movements you cannot control. Dystonia can be focal—like writer’s cramp or cervical dystonia—or more widespread. You feel stuck and uncertain how to regain ease and function.
Movement Does Not Work the Way You Want
Dystonia disrupts normal motor control. Even simple actions—reaching, writing, speaking—can become challenging. Traditional interventions help some people, but others still struggle to feel in command of their body. You are searching for approaches that go beyond symptom suppression, aiming instead at functional coordination and integration.
Common Types of Dystonia
Dystonia is a broad term that covers a variety of movement disorders characterized by involuntary muscle contractions causing twisting, repetitive movements, or abnormal postures. These contractions can affect one part of the body, several regions, or be generalized throughout. Understanding the common types helps clarify symptoms and guides treatment strategies.
1. Focal Dystonia
Focal dystonia affects a single body region. It is the most common form and often task-specific. Examples include:
- Cervical dystonia (spasmodic torticollis): Involuntary contractions of neck muscles cause the head to twist or tilt abnormally.
- Blepharospasm: Excessive blinking or eyelid spasms, sometimes causing functional blindness.
- Writer’s cramp: Affects the hand and forearm during writing or fine motor tasks.
2. Segmental Dystonia
Segmental dystonia involves two or more adjacent parts of the body. For example, cervical dystonia may spread to the shoulder or face, affecting multiple areas in close proximity.
3. Generalized Dystonia
This form affects multiple body regions, often including the trunk and legs. It is more disabling and usually starts in childhood or adolescence. Generalized dystonia can be primary (genetic or idiopathic) or secondary to other neurological conditions.
4. Hemidystonia
Hemidystonia involves one side of the body, typically caused by brain lesions such as stroke or injury affecting the basal ganglia or thalamus on one side.
5. Paroxysmal Dystonia
Characterized by sudden, brief episodes of dystonia triggered by specific factors such as movement, stress, or sudden noises. Between episodes, individuals have normal motor function.
Why Knowing the Type Matters
Each type of dystonia can vary in severity and treatment approach. For example, botulinum toxin injections work well for focal dystonias like cervical dystonia or blepharospasm but may be less practical for generalized forms. Functional neurology approaches, including those used in chiropractic neurology, often tailor sensory-motor retraining depending on the affected regions and symptoms.
Understanding your dystonia type helps create a targeted plan for managing symptoms and improving quality of life.
Chiropractic Neurology as a Movement‑Focused Ally
Chiropractic neurology is not about pain relief alone. It is a specialty that blends neuro-functional input and movement-based strategies to help re-establish normal coordination. The aim is to support motor control, sensory processing, posture, and ocular coordination—especially helpful in movement disorders like dystonia.
What Happens in the Brain During Dystonia
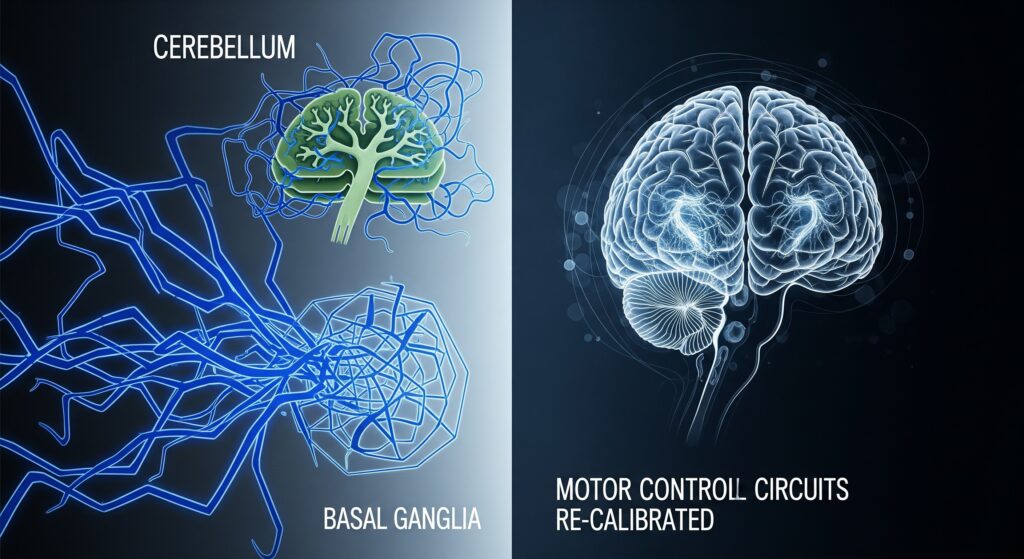
Research now understands dystonia as a network disorder, not just a problem in one brain region. The following areas are key:
- Basal Ganglia (particularly striatum and globus pallidus): These nuclei normally suppress unintended movements. In dystonia, that inhibitory gating is impaired, allowing excessive, involuntary muscle activation.
- Cerebellum: Traditionally linked to balance and coordination, new evidence shows its crucial role in dystonia—especially through disruption of cerebellar Purkinje cell function and cerebello‑basal ganglia circuits.
- Thalamo-cortical and cortico-basal ganglia loops: These overlapping feedback circuits coordinate motor commands. When disrupted, they lead to sustained abnormal activations and poor motor control.
- Brainstem and spinal inhibition circuits: Reflex suppression is often reduced in dystonia, contributing to co‐contraction and overflow into unintended muscle groups.
In short, dystonia reflects disrupted sensorimotor integration across basal ganglia, cerebellum, thalamus, cortex, brainstem, and spinal circuits. This network dysfunction explains why simple movements become distorted and persistent.
How Chiropractic Neurology May Support Dystonia
Although direct clinical trials are limited, case-based evidence suggests that neuro‑functional approaches may help reduce symptom severity in focal dystonia:
- In a case of cervical dystonia, clinicians applied vibration input and eye-movement integration—without medication or invasive procedures—and observed measurable reduction in symptom severity.
- Another report described a patient with persistent torticollis who improved following non-pharmacological neuro‑functional care involving structured sensory‑motor input.
Clinicians using functional neurology may emphasize eye–hand coordination, head/neck proprioceptive input, and sensory retraining to recalibrate motor outputs. A qualitative example described the use of eye movements targeting midbrain structures and cerebellar coordination drills to reshape cortical mapping—reporting long-term symptomatic improvement.
Putting It All Together: A Coordinated Approach
- Motor network engagement: Precise sensory-motor input—especially to the neck, eyes, and posture—may help recalibrate the cerebello‑basal ganglia loops contributing to dystonic postures.
- Sensory retraining: Techniques aimed at improving how sensory feedback is processed can help reduce co-contraction and overflow in unwanted muscles.
- Functional brain mapping exercises: Coordination targets specific brain regions (e.g. superior colliculus, globus pallidus) to promote neuroplastic changes in movement circuits.
This approach does not rely on high-force techniques, and though evidence is limited, it aligns with what is known about dystonia’s network pathology.
Common Medical Treatments
- Botulinum toxin injections for focal dystonias (e.g. cervical, blepharospasm). These reduce muscle contractions by chemically inhibiting affected motor neurons.
- Medications such as anticholinergics (trihexyphenidyl), baclofen, or benzodiazepines can help reduce involuntary muscle activity, though side‑effects may limit use.
- Deep brain stimulation (DBS) targeted at the globus pallidus internus (GPi) can offer significant improvements in medication-resistant or generalized dystonia, although effects may appear over weeks to months.
If you or someone you love is suffering from dystonia and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed References
- Albanese, A., Bhatia, K., Bressman, S. B., DeLong, M. R., Fahn, S., Fung, V. S. C., … & Teller, J. K. (2013). Phenomenology and classification of dystonia: A consensus update. Movement Disorders, 28(7), 863–873. https://doi.org/10.1002/mds.25475
- Bragg, D. C., Sharma, N., & Ozelius, L. J. (2021). Emerging pathways of dystonia pathophysiology: Insights from human and animal genetics. Brain Structure and Function, 226, 1011–1022. https://doi.org/10.1007/s00429-021-02299-y
- LeDoux, M. S. (2013). Animal models of dystonia: Lessons from a mutant rat. Neurobiology of Disease, 62, 306–312. https://doi.org/10.1016/j.nbd.2013.09.006
- Neychev, V. K., Gross, R. E., Lehericy, S., Hess, E. J., & Jinnah, H. A. (2011). The functional neuroanatomy of dystonia. Neurobiology of Disease, 42(2), 185–201. https://doi.org/10.1016/j.nbd.2011.01.026
- Samotus, O., Lee, J., Jog, M. (2014). Personalized low-frequency stimulation effectively treats focal hand dystonia in musicians. Frontiers in Neurology, 5, 122. https://doi.org/10.3389/fneur.2014.00122
- Tanabe, L. M., Kim, C. E., & Alagem, N. (2020). Primary dystonia: Molecules and mechanisms. Nature Reviews Neurology, 16, 256–268. https://doi.org/10.1038/s41582-020-0345-7
