The Pain That Does Not Make Sense
You sprained your ankle—or maybe you broke a bone in your hand. Weeks go by, and the pain not only lingers but grows. It burns. It throbs. The skin around it changes color, becomes swollen or shiny. The slightest breeze feels like fire, and you feel like a prisoner inside your own body. Friends and doctors say it is “just healing,” but you know something is deeply wrong.
Complex Regional Pain Syndrome (CRPS) is a condition that does not follow the rules. It hijacks the nervous system and often leaves patients feeling hopeless, misunderstood, and desperate for answers.
At Georgia Chiropractic Neurology Center, we understand that pain like this is not just about tissues or injuries—it is about the brain, the maps it holds, and the messages it sends. There is a path forward.
What Is Complex Regional Pain Syndrome (CRPS)?
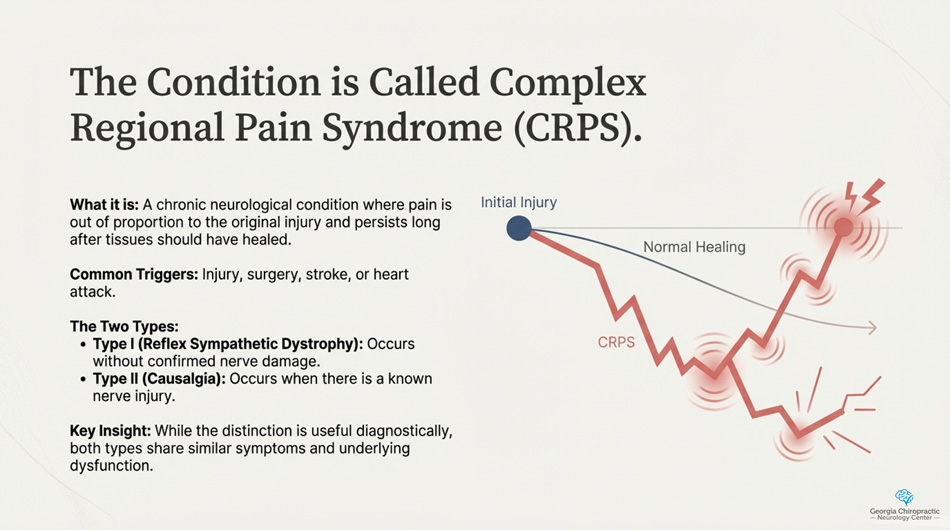
CRPS is a chronic neurological condition most commonly triggered by an injury, surgery, stroke, or heart attack. What makes it unique is that the pain is often out of proportion to the original injury and persists long after tissues should have healed.
There are two types:
- Type I (formerly Reflex Sympathetic Dystrophy) – Occurs without confirmed nerve damage.
- Type II (formerly Causalgia) – Occurs when there is a known nerve injury.
While the distinction is useful diagnostically, both types share similar symptoms and underlying dysfunction.
Symptoms: When the Brain Feels Pain Even Without Injury
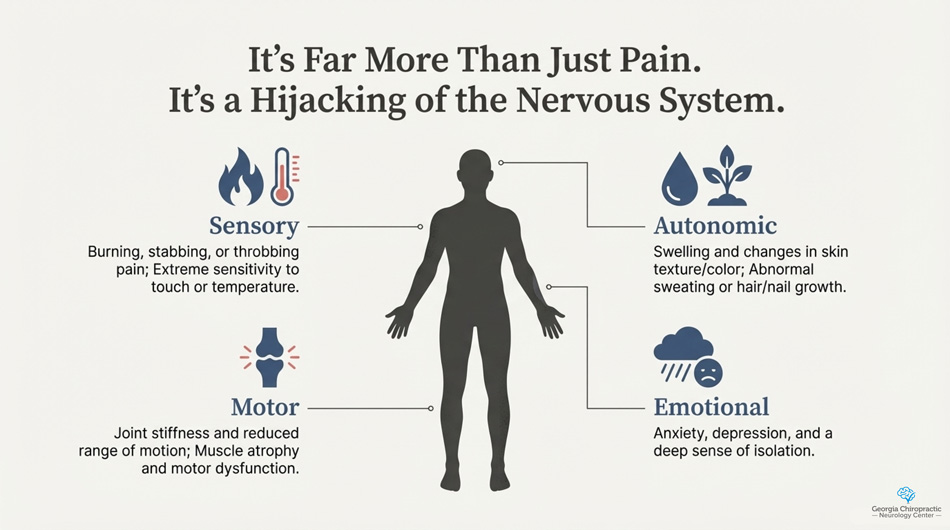
CRPS symptoms go beyond ordinary pain. They include:
- Burning, stabbing, or throbbing pain
- Extreme sensitivity to touch or temperature
- Swelling and changes in skin texture or color
- Joint stiffness and reduced range of motion
- Abnormal sweating or hair/nail growth
- Muscle atrophy and motor dysfunction
- A strong emotional toll—anxiety, depression, and isolation
It typically affects a limb (arm, leg, hand, or foot) and may spread to other areas over time. Many patients describe a deep sense of disconnect from the affected body part—like it no longer belongs to them.
What Causes CRPS?
The exact cause of CRPS is still being studied, but we know several factors are involved:
- Nervous system dysfunction – especially of the sympathetic nervous system.
- Maladaptive neuroplasticity – where the brain reorganizes itself in a way that reinforces pain.
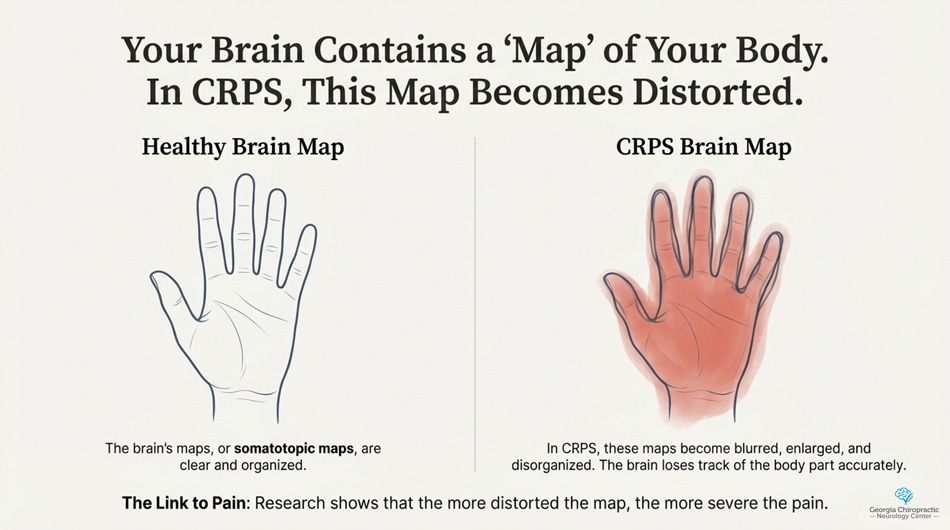
- Distorted somatotopic maps – the brain’s internal body maps become blurred or inaccurate.
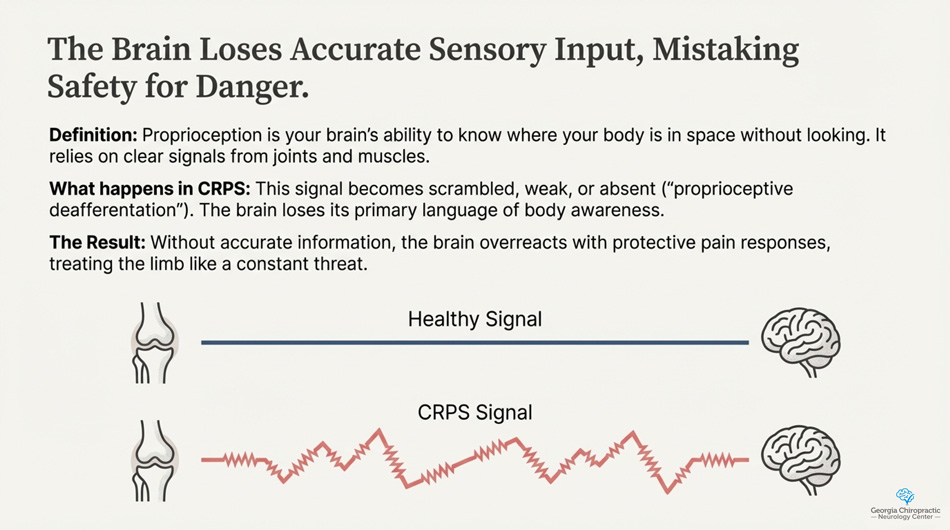
- Proprioceptive deafferentation – meaning the brain loses accurate sensory input from the body.
- Inflammatory and immune changes – local inflammation and possible involvement of mast cells and cytokines.
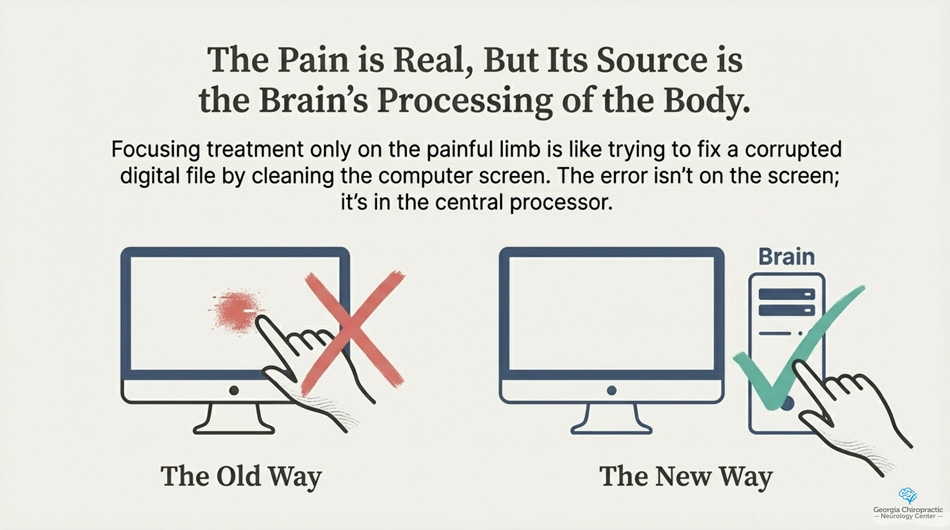
This means CRPS is not just a “pain condition”—it is a neurological syndrome where the pain is real, but the source is the brain’s processing of the body, not just the tissue itself.
The Impact on Daily Life
CRPS can be life-altering. The pain and movement restrictions often prevent people from working, enjoying social time, sleeping, or even dressing and feeding themselves. The unpredictability and severity of flare-ups create emotional strain, and the lack of visible injury can make it hard for others to understand.
The longer CRPS persists, the more likely maladaptive changes in the brain will cement. This is why early and neuro-centered intervention is essential.
Conventional Medical Treatment Options
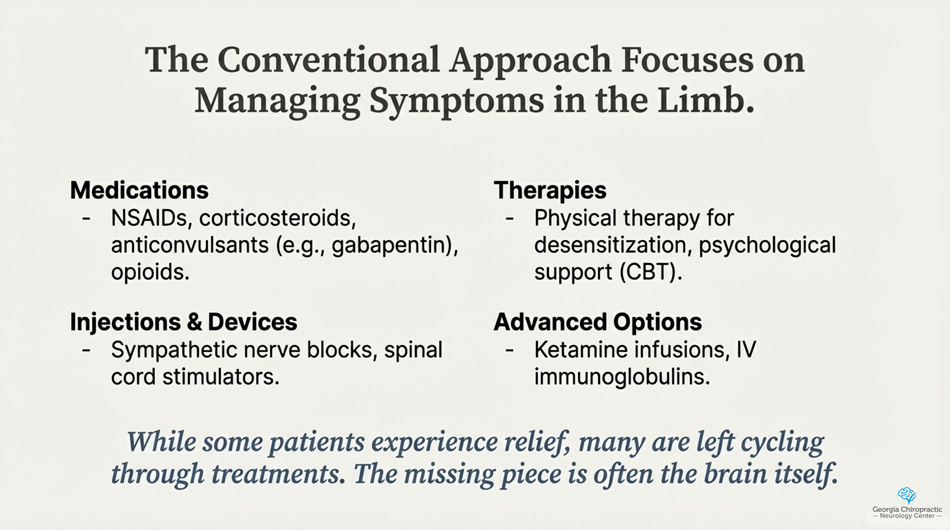
The medical world approaches CRPS with a combination of strategies. These include:
- Medications – including NSAIDs, corticosteroids, anticonvulsants (e.g., gabapentin), antidepressants, bisphosphonates, and opioids.
- Sympathetic nerve blocks – used to reduce autonomic nervous system overactivity.
- Spinal cord stimulators – implanted devices that disrupt pain signaling.
- Physical therapy – focused on desensitization and restoring movement.
- Psychological support – cognitive behavioral therapy is often recommended due to the emotional burden.
- Ketamine infusions or IV immunoglobulins – used in some treatment-resistant cases.
While some patients experience relief, others are left cycling through treatments with little success. The missing piece is often the brain itself—how it maps, feels, and moves the body.
A Chiropractic Neurology Approach: Rewiring Pain Through Brain-Based Care
At Georgia Chiropractic Neurology Center, we take a different approach. Rather than focusing solely on the site of pain, we look at the entire sensorimotor system, with a particular focus on proprioception and somatotopic mapping.
Proprioception: The Language of Body Awareness
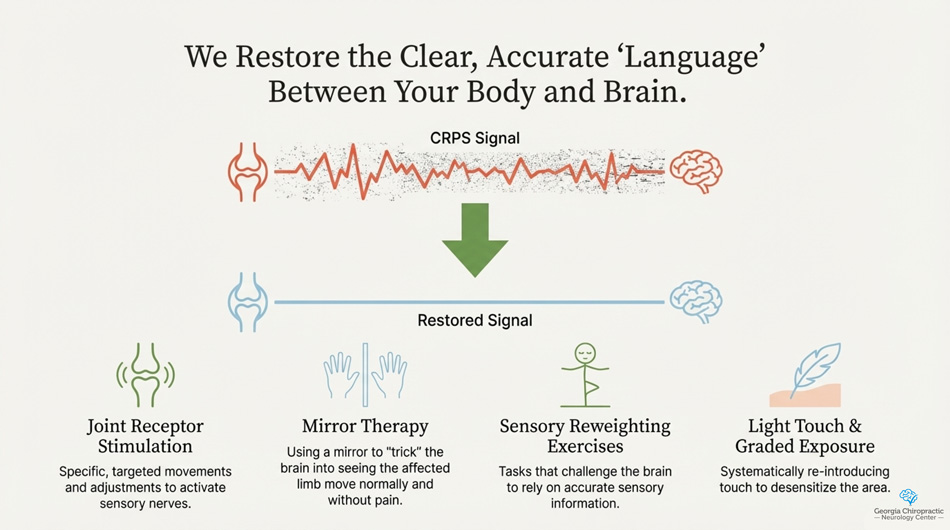
Proprioception is your brain’s ability to know where your body is in space without looking. It relies on signals from joints, muscles, and fascia to tell the brain, “Here is your arm, it is bent, and it is safe.” In CRPS, this signal becomes scrambled or absent, which can cause the brain to overreact with protective pain responses.
Patients with CRPS often have impaired proprioception on the affected side. Their body no longer feels “normal” or safe, and the brain treats it like a danger zone—even after the injury is long gone.
Restoring proprioceptive input is foundational in our approach. We use techniques such as:
- Joint receptor stimulation
- Mirror therapy and visual-proprioceptive retraining
- Sensory reweighting exercises
- Vibration or mechanoreceptor stimulation
- Light touch and graded exposure tasks
Somatotopic Maps: When the Brain Loses Track of the Body
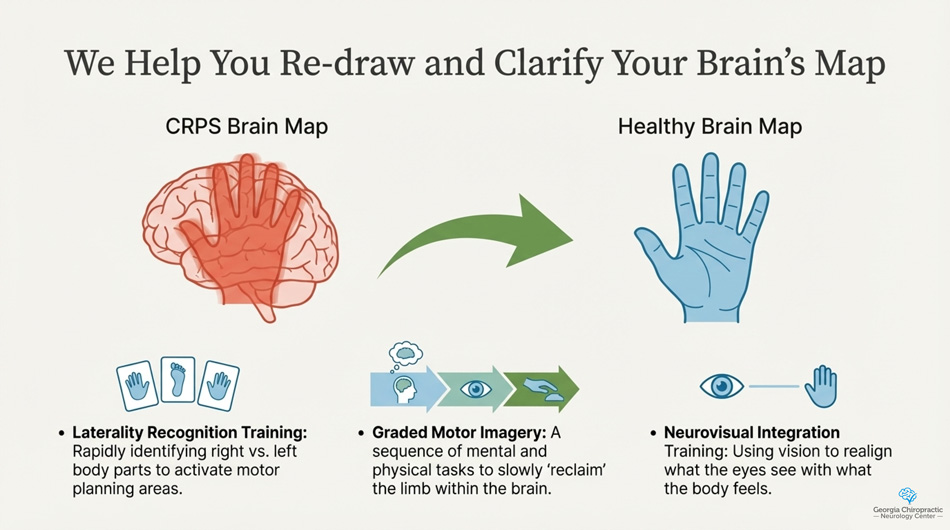
The brain contains maps—organized areas that correspond to body regions. These are called somatotopic maps, and they reside primarily in the primary somatosensory cortex (S1). In CRPS, these maps become distorted. For example, a person’s brain may enlarge the representation of their painful hand or blur the boundaries between fingers. This leads to pain, sensory mismatch, and even motor dysfunction.
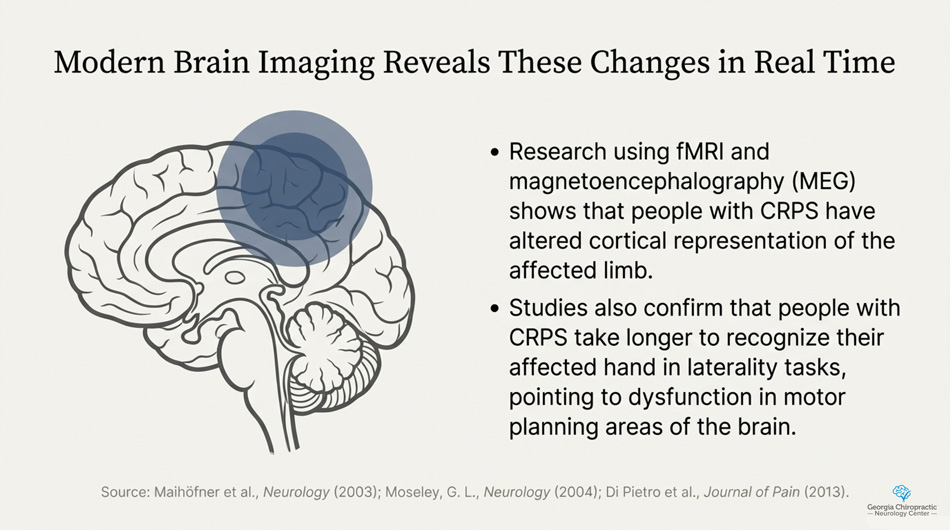
Research using fMRI and magnetoencephalography (MEG) shows that people with CRPS often have altered cortical representation of the affected limb. The more distorted the map, the more severe the pain.
We aim to restore these maps using:
- Neurovisual integration training – to realign visual and proprioceptive information.
- Laterality recognition training – identifying right vs. left body parts to activate motor planning areas.
- Graded motor imagery – a sequence of tasks that helps “reclaim” the limb within the brain.
- Neuroplasticity-based exercises – that challenge sensory and motor systems simultaneously.
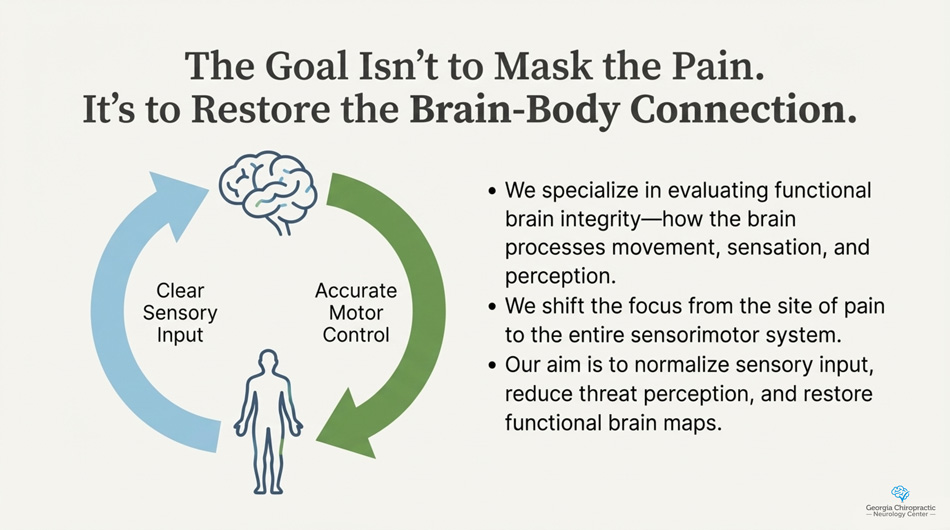
Why Chiropractic Neurology Works for CRPS
Chiropractic neurologists specialize in evaluating functional brain integrity—especially how the brain processes movement, sensation, and perception. Rather than masking pain, our goal is to normalize sensory input, reduce threat perception, and restore functional brain-body connections.
Your brain’s ability to interpret safety vs. danger is at the core of CRPS. By correcting the sensory distortions and rebuilding somatotopic accuracy, the brain can re-learn that the body is not in crisis—and pain can recede.
Multimodal and Individualized Care
No two CRPS patients are the same, which is why our care plans are highly individualized. We combine:
- Functional neurological examination
- Neuroplasticity-based rehab
- Proprioceptive stimulation
- Vestibular and visual integration
- Brain-based movement retraining
- Nutritional and anti-inflammatory guidance
- Emotional regulation techniques (e.g., vagal tone training)
Our aim is not to “treat the limb,” but to retrain the brain that governs it.
Hope Is Real. Healing Is Possible.
If you have been living with Complex Regional Pain Syndrome, you may have been told to “just live with it.” You may have tried medication after medication, undergone injections or surgery, and still found no relief. But there is another path—one that respects the complexity of your nervous system and works with your brain’s ability to change.
At Georgia Chiropractic Neurology Center, we believe that pain is not just a symptom—it is a message. And with the right tools, we can help you rewire the message and restore control over your body and your life.
If you or someone you love is suffering from complex regional pain syndrome and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed References
- Afrin, L. B., Butterfield, J. H., & Raithel, M. (2016). Presentation, diagnosis, and management of mast cell activation syndrome. Hematology/Oncology Clinics of North America, 30(1), 179–193. https://doi.org/10.1016/j.hoc.2015.09.011
- Molderings, G. J., Haenisch, B., Brettner, S., & Homann, J. (2011). Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options. Journal of Hematology & Oncology, 4(1), 10. https://doi.org/10.1186/1756-8722-4-10
- Theoharides, T. C., & Kalogeromitros, D. (2006). The critical role of mast cells in allergy and inflammation. Annals of the New York Academy of Sciences, 1088(1), 78–99. https://doi.org/10.1196/annals.1366.052
- Weinstock, L. B., Brook, J. B., Myers, T. L., Goodman, B., & Afrin, L. B. (2021). Mast cell activation symptoms are prevalent in Long-COVID. International Journal of Infectious Diseases, 112, 217–226. https://doi.org/10.1016/j.ijid.2021.08.016