Cervical dystonia (also known as spasmodic torticollis) is a complex neurological disorder characterized by involuntary, sustained, or intermittent contractions of the neck muscles. These contractions often lead to abnormal head postures, tremors, and significant functional impairment. Despite being classified as a movement disorder, its pathophysiology extends well beyond muscle activity, involving disruptions in sensory processing, cortical excitability, and motor planning.
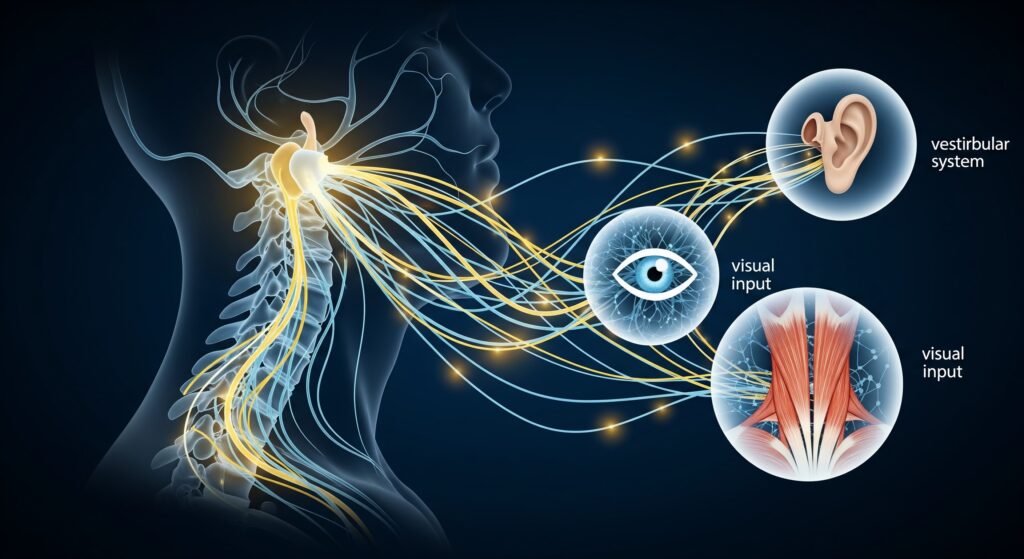
Chiropractic neurology offers a unique, non-invasive framework for addressing the multifaceted dysfunctions associated with cervical dystonia. Rather than focusing solely on musculoskeletal output, this approach considers the deep interplay between the sensory systems—vestibular, visual, proprioceptive, and cutaneous—and their influence on motor control.
This article explores current insights into the neurophysiology of cervical dystonia and outlines a multimodal rehabilitative strategy rooted in chiropractic neurology, with particular emphasis on vestibular rehabilitation. We also examine how the evaluation and modulation of cutaneous-muscular reflexes may play a supportive role in clinical outcomes.
Understanding the Neurological Complexity of Cervical Dystonia
Cervical dystonia is increasingly recognized as a disorder of sensorimotor integration rather than isolated hyperactivity of cervical muscles. Neuroimaging and electrophysiological studies implicate dysfunctions in basal ganglia-thalamocortical circuits, sensorimotor cortex abnormalities, cerebellar involvement, and disrupted brainstem integration.
Common features in patients with cervical dystonia include:
- Altered temporal and spatial discrimination thresholds
- Decreased cortical inhibition (measured by transcranial magnetic stimulation)
- Abnormal sensory trick (geste antagoniste) phenomena
- Dysregulated proprioceptive and vestibular input processing
These findings suggest that the central nervous system struggles to correctly interpret sensory information and generate coordinated motor output. Therefore, therapeutic strategies that aim to restore or retrain multisensory processing may provide more lasting improvements than those targeting motor symptoms alone.
The Role of Chiropractic Neurology in Sensorimotor Rehabilitation
Chiropractic neurology applies principles from neurophysiology, neuroplasticity, and clinical neuroscience to assess and support the nervous system’s function. When applied to cervical dystonia, it shifts the therapeutic lens away from symptomatic muscle relaxation and toward modulation of aberrant central processing, especially within the vestibular, visual, and somatosensory domains.
Rather than using a single intervention, chiropractic neurologists often employ multi-modal strategies including:
- Vestibular rehabilitation therapy (VRT)
- Sensorimotor integration training
- Eye-head coordination drills
- Postural and balance retraining
- Cutaneous and proprioceptive feedback techniques
These interventions are tailored to the individual’s neurological profile, based on functional assessment rather than structural imaging alone.
Vestibular Rehabilitation as a Foundational Strategy
The vestibular system is closely integrated with cervical motor control via the vestibulocollic reflex (VCR), vestibulo-ocular reflex (VOR), and cervico-ocular reflex (COR). In healthy individuals, these reflexes maintain head and gaze stability during movement. In cervical dystonia, research has shown that these reflexes may be dysregulated, contributing to abnormal head posturing and difficulty with spatial orientation.
Vestibular rehabilitation therapy (VRT), a mainstay in neurological rehabilitation, offers substantial benefits when applied in a chiropractic neurology framework.
Core Components of VRT in Cervical Dystonia Include:
- Gaze Stabilization Exercises
Designed to recalibrate the VOR, these exercises require patients to fix their gaze on a target while moving the head in controlled patterns. Progressions include increasing speed, range of motion, and complexity of visual backgrounds. - Head-Eye Coordination Drills
These exercises challenge the brain’s ability to integrate visual, vestibular, and cervical proprioceptive input. For example, target tracking with delayed or predictive saccades combined with head movement. - Balance and Postural Challenges
Incorporating unstable surfaces, narrow bases of support, and altered visual environments (eyes closed, visual flow) helps engage vestibulospinal reflexes and reinforces sensorimotor integration. - Habituation and Repetition
Gradual exposure to movements or stimuli that typically provoke dystonic responses can, over time, reduce sensitivity and recalibrate neural responses.
The key in VRT is neuroplastic adaptation: by repeatedly activating healthy vestibular-cervical circuits, the brain may downregulate abnormal patterns and re-establish more functional motor outputs.
Supporting Somatosensory Integration in Clinical Practice
While vestibular input plays a central role, somatosensory feedback from skin, joints, and muscles is equally essential in regulating posture and movement. Research indicates that individuals with cervical dystonia often display impaired proprioceptive acuity and altered cutaneous discrimination, further contributing to maladaptive motor patterns.
Chiropractic neurologists frequently assess and train these systems using techniques such as:
- Joint position sense testing
- Vibration and tactile threshold assessments
- Surface EMG or biofeedback for muscle activation awareness
- Sensory-motor matching tasks (e.g., mirror feedback or limb-matching exercises)
Through repeated exposure and sensory re-weighting, patients can learn to improve accuracy in sensory perception and recalibrate motor responses.
The Role of Cutaneous-Muscular Reflexes
One specific, yet underutilized, aspect of somatosensory integration is the cutaneous-muscular reflex (CMR)—a spinal reflex in which cutaneous stimulation of the skin results in a localized muscle response.
In the cervical region, stimulation of dermatomes (such as C3–C5) may evoke responses in the deep cervical flexors, trapezius, or levator scapulae. These reflexes are polysynaptic, influenced by both ascending sensory input and descending cortical modulation. Dysregulation may result in diminished or excessive muscle responsiveness, both of which are features observed in cervical dystonia.
Clinical Application of CMRs:
- Assessment
Light touch, brush, or vibration is applied to cervical dermatomes while monitoring for immediate muscle responses. Differences between sides or delayed responses may indicate dysfunctional integration. - Facilitation Techniques
Cutaneous stimulation can be paired with intentional muscle activation to reinforce appropriate neuromuscular patterns. For example, stroking the skin overlying C4 while cueing the patient to gently engage the deep neck flexors. - Neuromodulation
Repeated cutaneous stimulation may influence spinal excitability and cortical plasticity. This could potentially improve reflex timing and muscle tone regulation over time.
Though not a standalone intervention, CMR-based techniques complement broader sensorimotor strategies and support the goal of re-establishing reflexive control of the cervical spine.
Advantages of a Multimodal Chiropractic Neurology Approach
Chiropractic neurology’s strength lies in its ability to combine detailed neurological assessment with tailored, non-invasive interventions. For individuals with cervical dystonia, this means a care model that is:
- Neurophysiologically grounded
Interventions are designed to engage known pathways (e.g., VOR, CMR, proprioceptive reflex arcs). - Individualized
Based on functional deficits identified during neurological examination, not generic protocols. - Non-invasive and active
Patients are active participants in their care, enhancing neuroplastic outcomes through repetition and engagement. - Complementary to other care
These methods do not interfere with pharmacological or surgical treatments but can improve outcomes and possibly reduce reliance on more invasive procedures.
If you or someone you love is suffering from cervical dystonia and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed References
- Zehr, E. P., & Stein, R. B. (1999). What functions do reflexes serve during human locomotion? Progress in Neurobiology, 58(2), 185–205.
— Discusses the functional role of spinal reflexes in movement control, including cutaneous-muscular responses. - Popa, T., Russo, M., Meunier, S. (2010). Long-lasting inhibition of cerebellar output. Brain, 133(4), 1174–1187.
— Highlights cerebellar contributions to sensorimotor integration in dystonia. - Nashner, L. M., & McCollum, G. (1985). The organization of human postural movements. Behavioral and Brain Sciences, 8(1), 135–172.
— A foundational text on multisensory integration for postural control. - Stubbs, D. A., Mrachacz-Kersting, N., & Lamont, E. V. (2011). Cutaneous reflex excitability during locomotor-like movement in humans. Journal of Neurophysiology, 105(3), 1464–1474.
— Demonstrates the adaptability of cutaneous reflexes under different sensorimotor conditions. - **Avanzino, L., Tinazzi, M., Ionta, S., Fiorio
