You Were Made to Feel Steady
We take balance for granted—until it is gone. Whether it is a sudden wave of dizziness while turning your head, a vague sense of disequilibrium in crowded environments, or full-blown vertigo, dysfunction in the vestibular system can turn everyday life into a minefield. For many, these symptoms come with a frustrating lack of answers or relief.
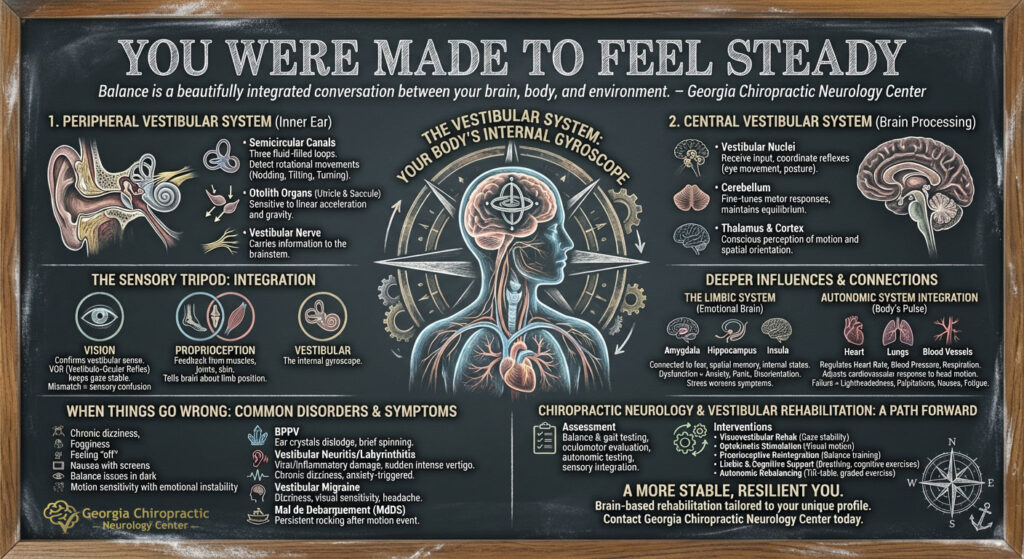
At Georgia Chiropractic Neurology Center, we understand that balance is more than just inner ear function—it is a beautifully integrated conversation between your brain, body, and environment. Our goal is to help you understand how this system works, how it breaks down, and how we can support it through cutting-edge neurological rehabilitation.
Understanding the Vestibular System
The vestibular system is your body’s internal gyroscope. It tells your brain where your head is in space, whether you’re moving or still, and whether you are upright or tilted. It does all this subconsciously, in real time, allowing you to read in a moving car, walk in a straight line, or stand on one foot.
Let’s break it down into its two major parts:
1. The Peripheral Vestibular System
Located in the inner ear, this portion consists of:
- The semicircular canals – Three fluid-filled loops that detect rotational movements of the head.
- The otolith organs (utricle and saccule) – Sensitive to linear acceleration and gravity.
- The vestibular nerve – Carries information from these structures to the brainstem.
Each semicircular canal corresponds to a different plane of motion: nodding, tilting, and turning your head. When you move, fluid in the canals shifts and deflects hair cells, sending mechanical signals to the brain about angular movement. The utricle and saccule track shifts like leaning forward or accelerating in a car.
2. The Central Vestibular System
Once the signals from your ears reach the brainstem, they are processed by several critical structures:
- Vestibular nuclei in the brainstem – These nuclei receive input from both ears and help coordinate reflexes like eye movement and posture.
- The cerebellum – Fine-tunes motor responses and maintains equilibrium.
- The thalamus and cortex – Contribute to conscious perception of motion and spatial orientation.
Visual and Proprioceptive Integration
The vestibular system does not act alone. It works hand-in-hand with two other major sensory systems:
1. Vision
Visual input confirms what the vestibular system senses. The brain compares these two sources of information to create a stable picture of the world. For example, if you turn your head to the right, your eyes automatically shift left (via the vestibulo-ocular reflex or VOR) to keep your gaze stable. When the visual and vestibular systems do not agree, you are experiencing sensory mismatch and you feel disoriented or nauseous—think about motion sickness or trying to walk after getting off a moving boat.
2. Proprioception
Proprioceptive feedback comes from muscles, joints, and skin, telling your brain about the position of your limbs and body. The cerebellum plays a key role in integrating this with vestibular input. For instance, if your feet feel the ground tilting, but your inner ear does not confirm this, the mismatch causes balance problems.
Together, these three systems form a sensory tripod. If one leg becomes weak, the other two compensate—but only to a point.
The Deeper Influence: The Limbic System
Many people are surprised to learn that the vestibular system is tightly connected to the limbic system—the emotional brain.
Vestibular nuclei have direct connections to:
- The amygdala – governing fear and emotional tagging
- The hippocampus – involved in spatial memory and navigation
- The insula – which interprets internal states of the body
This explains why vestibular dysfunction often causes anxiety, panic, or feelings of disorientation even in emotionally neutral settings. It also explains why emotional stress can worsen vestibular symptoms. A dysregulated limbic system can upregulate perceived motion or dizziness even in the absence of true dysfunction.
The Body’s Pulse: Autonomic System Integration
The vestibular system also ties into autonomic regulation, especially in the context of orthostatic tolerance and head motion.
Vestibular nuclei send signals to centers in the brainstem that regulate:
- Heart rate
- Blood pressure
- Respiration
When you stand up or move your head quickly, the vestibular system helps adjust your cardiovascular responses. If this fails, you may experience symptoms of dysautonomia, such as:
- Lightheadedness
- Heart palpitations
- Nausea
- Fatigue
This integration is key for diagnosing and treating conditions like POTS (Postural Orthostatic Tachycardia Syndrome), vestibular migraines, and mal de debarquement syndrome, where both balance and autonomic dysfunction overlap.
When Things Go Wrong
Vestibular dysfunction does not always mean vertigo. Symptoms can range widely and be subtle:
- Chronic dizziness or fogginess
- Feeling “off” in crowded stores or on uneven ground
- Nausea while scrolling on a screen
- Balance issues when walking in the dark
- Emotional instability in conjunction with motion sensitivity
Common vestibular disorders include:
- Benign Paroxysmal Positional Vertigo (BPPV) Small crystals in the inner ear dislodge and disrupt fluid movement in the canals, leading to brief spinning sensations with head movement.
- Vestibular Neuritis/Labyrinthitis Viral or inflammatory damage to the vestibular nerve or inner ear, causing sudden, intense vertigo, often accompanied by imbalance.
- Persistent Postural-Perceptual Dizziness (PPPD) Chronic dizziness and unsteadiness, often triggered by anxiety or sensory overload, frequently seen post-infection or post-vestibular event.
- Vestibular Migraine Characterized by dizziness, visual motion sensitivity, and headache, often without classic vertigo.
- Mal de Debarquement Syndrome (MdDS) A persistent feeling of rocking or swaying after disembarking from a cruise, plane, or motion event—associated with failure to reintegrate vestibular input.
Chiropractic Neurology and Vestibular Rehabilitation
At Georgia Chiropractic Neurology Center, we use a functional neurology model to address vestibular dysfunction. This includes evaluating how each system—vestibular, visual, proprioceptive, limbic, and autonomic—contributes to your symptoms and tailoring a precise rehabilitation plan.
Assessment Includes:
- Comprehensive balance and gait testing
- Oculomotor evaluations (eye movement tracking, videonystagmography testing)
- Autonomic function testing (e.g., heart rate variability, orthostatic challenges)
- Sensory integration and cognitive assessments
Interventions May Include:
- Visuovestibular Rehabilitation Exercises that retrain eye-head coordination and VOR. For example, gaze stability training involves focusing on a fixed point while moving your head side to side.
- Optokinetic Stimulation Visual motion exercises that desensitize the brain to movement sensitivity and recalibrate midbrain and cerebellar processing.
- Proprioceptive Reintegration Balance training using foam surfaces, tilt boards, or joint loading to enhance proprioceptive input and cerebellar modulation.
- Limbic and Cognitive Support Breathing exercises, cognitive exercises, and limbic system modulation (through midline cerebellar activation or frontal lobe engagement) help downregulate overactive threat responses.
- Autonomic Rebalancing Tilt-table training, graded exercise, and vestibulo-autonomic exercises support orthostatic tolerance and systemic regulation.
Vestibular rehabilitation is not a one-size-fits-all approach. For some patients, starting with visual rehab is essential. For others, limbic desensitization must come first before the brain can tolerate motion again.
The Outcome: A More Stable, Resilient You
A healthy vestibular system is foundational to feeling present in your body and in the world. When this system falters, it affects more than just balance—it can unravel your sense of emotional and physiological safety. But with precise, brain-based rehabilitation tailored to your unique sensory profile, your brain can learn to trust itself again.
If you have been living with unexplained dizziness, motion sensitivity, anxiety, or imbalance, you do not have to suffer in silence. There is a path forward—and we are here to walk it with you.
If you or someone you love is suffering from a vestibular disorder and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed References
- Balaban, C. D., & Thayer, J. F. (2001). Neurological bases for balance-anxiety links. Journal of Anxiety Disorders, 15(1-2), 53–79. https://doi.org/10.1016/S0887-6185(00)00041-6
- Dieterich, M., & Brandt, T. (2015). The bilateral central vestibular system: its pathways, functions, and disorders. Annals of the New York Academy of Sciences, 1343(1), 10–26. https://doi.org/10.1111/nyas.12569
- Staab, J. P., & Ruckenstein, M. J. (2003). Chronic dizziness and anxiety: Effect of course of illness on treatment outcome. Archives of Otolaryngology–Head & Neck Surgery, 129(5), 547–552. https://doi.org/10.1001/archotol.129.5.547
- Yates, B. J., Miller, A. D., & Lucot, J. B. (1998). Physiological basis and pharmacology of motion sickness: An update. Brain Research Bulletin, 47(5), 395–406. https://doi.org/10.1016/S0361-9230(98)00116-3
