When Your Body Cannot Stabilize
Have you ever felt like your body just does not hold itself together the way it should—like your joints move too far, your heart races just from standing up, or you feel faint without warning? These symptoms can feel random and overwhelming, leaving you without a clear diagnosis or treatment plan. Maybe you have been told you are “just anxious,” or your tests all come back “normal,” even when your daily life is anything but.
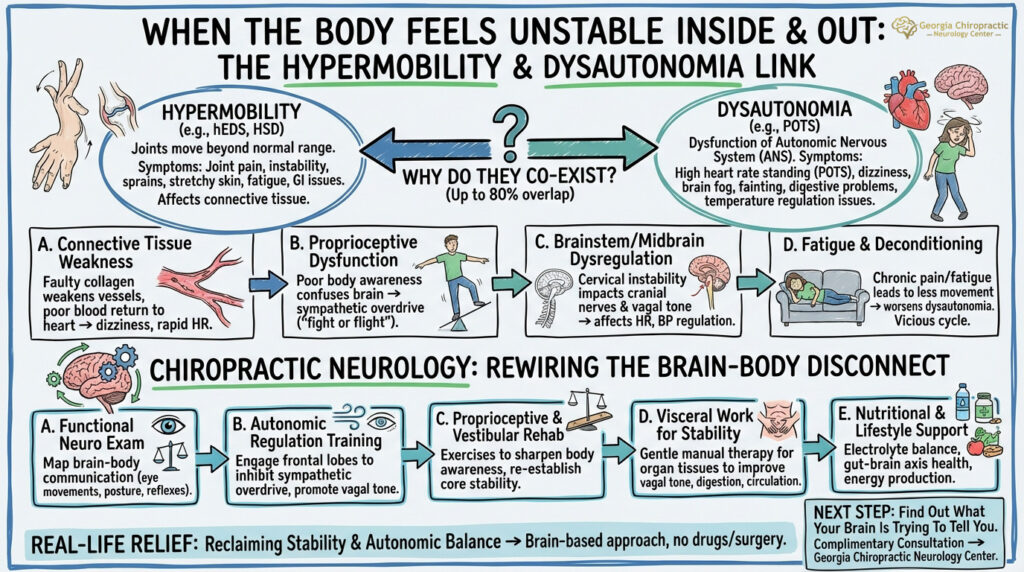
If this sounds familiar, you are not alone. For many people—especially young women—there is a hidden link between two often misunderstood conditions: hypermobility disorders and dysautonomia. While each condition presents its own challenges, they frequently occur together in a complex interplay of structure and function. Chiropractic neurology offers a unique, whole-brain approach to treating these intersecting disorders without drugs or surgery.
What Is Hypermobility?
 Hypermobility refers to a condition where joints move beyond the normal range of motion. While many people may be naturally flexible or “double-jointed,” pathological hypermobility goes beyond flexibility—it can affect connective tissue throughout the body, leading to widespread symptoms.
Hypermobility refers to a condition where joints move beyond the normal range of motion. While many people may be naturally flexible or “double-jointed,” pathological hypermobility goes beyond flexibility—it can affect connective tissue throughout the body, leading to widespread symptoms.
The most well-known hypermobility disorder is Ehlers-Danlos Syndrome (EDS), particularly the hypermobile type (hEDS). Though hEDS has no identified genetic marker yet, other EDS subtypes (like vascular or classical EDS) are genetically confirmed and can be life-threatening.
Common symptoms of hypermobility disorders include:
- Joint pain and instability
- Frequent sprains, dislocations, or subluxations
- Soft or stretchy skin
- Poor wound healing
- Gastrointestinal issues
- Fatigue
EDS is estimated to affect 1 in 5,000 people, though hypermobility spectrum disorders (HSD) may affect many more due to underdiagnosis or misclassification (Rombaut et al., 2015).
What Is Dysautonomia?
Dysautonomia is a dysfunction of the autonomic nervous system (ANS)—the part of the nervous system that regulates involuntary body functions such as heart rate, blood pressure, digestion, and temperature regulation.
The most common subtype associated with hypermobility is Postural Orthostatic Tachycardia Syndrome (POTS). POTS is characterized by an abnormal increase in heart rate when standing up, often accompanied by dizziness, fatigue, and brain fog.
Other dysautonomic symptoms can include:
- Lightheadedness or fainting
- Nausea and digestive problems
- Cold hands and feet
- Exercise intolerance
- Anxiety-like symptoms
POTS affects an estimated 1–3 million people in the U.S., with 80–85% being women between the ages of 15 and 50 (Raj, 2013).
Why Do Hypermobility and Dysautonomia Co-Exist?
Studies suggest that up to 80% of individuals with hypermobile EDS also have symptoms of dysautonomia, most commonly POTS (Celletti et al., 2017). But why?
The connection lies in both structure and function:
A. Connective Tissue Weakness
- The same faulty collagen that causes joint instability in hypermobility can also weaken blood vessels. This leads to poor vascular tone, making it harder for the body to push blood back to the heart upon standing—causing the hallmark dizziness and rapid heart rate seen in POTS.
B. Proprioceptive Dysfunction
- People with hypermobility often have poor proprioception, or body awareness. This can confuse the brain’s sensory systems, leading to compensatory overactivation of the sympathetic nervous system (the “fight or flight” branch of the ANS).
C. Brainstem and Midbrain Dysregulation
- Structural instability in the cervical spine and fascial system may impact brainstem input and cranial nerve function. This, in turn, affects regulation of heart rate, blood pressure, and vagal tone—crucial to autonomic balance.
D. Fatigue and Deconditioning
- Chronic pain and fatigue from hypermobility lead to less movement and more deconditioning, which worsens dysautonomia. It is a vicious cycle that needs neurological and physical reconditioning—not just symptom suppression.
How Chiropractic Neurology Helps Rewire the Brain-Body Disconnect
At Georgia Chiropractic Neurology Center, we specialize in identifying how your brain and nervous system are functioning—not just what hurts or feels off. Our approach is based on neuroplasticity, the brain’s ability to adapt and rewire with the right stimuli.
Here is how we support patients struggling with both hypermobility and dysautonomia:
A. Comprehensive Functional Neurological Examination
We begin by mapping how your brain communicates with your body through balance, eye movements, posture, coordination, autonomic signs, and reflexes. Unlike standard neurological exams, we assess subtle changes in midbrain, cerebellar, and frontal lobe activity to create a customized care plan.
B. Autonomic Regulation Training
- Using neurocognitive therapy, we engage frontal lobe networks that help inhibit sympathetic overdrive and promote vagal tone (the parasympathetic “rest and digest” branch).
- This may include specific eye movement protocols, balance training, and breath work—all individualized to the patient’s neurological findings.
C. Proprioceptive and Vestibular Rehabilitation
People with hypermobility often have poor joint feedback to the brain. We use targeted vestibular and somatosensory exercises to sharpen proprioception and re-establish core stability.
This can help reduce compensatory overactivation of the ANS by giving the brain better body input, which in turn calms output.
D. Visceral Work for Autonomic Stability
The autonomic nervous system is deeply influenced by signals from the organs—especially those in the abdomen and pelvis. In hypermobility disorders, the connective tissues that support internal organs can become lax, allowing for slight shifts in organ position or tension on fascial attachments. This can send erratic signals to the brainstem and vagus nerve, intensifying dysautonomia symptoms.
Through gentle visceral manual therapy, we assess and release restrictions in the connective tissue surrounding the organs. This is particularly helpful for:
- Alleviating abdominal bloating and discomfort
- Improving vagal tone and digestion
- Reducing physical stress on the brainstem and spinal cord
- Supporting circulation to organs affected by poor vascular tone
By enhancing mobility and communication between the brain and internal organs, visceral work can restore a more accurate feedback loop to the autonomic nervous system—helping patients feel more grounded, stable, and regulated from the inside out.
E. Nutritional and Lifestyle Support
Nutritional deficiencies—especially in sodium, magnesium, and B vitamins—can exacerbate both hypermobility and dysautonomia symptoms.
We provide support for:
- Electrolyte balance (especially important in POTS)
- Gut-brain axis health
- Mitochondrial function and energy production
6. Real-Life Relief: Reclaiming Stability and Autonomic Balance
While both hypermobility disorders and dysautonomia can feel overwhelming and hard to diagnose, they are not untreatable. By viewing the body through a chiropractic neurology lens, we see the interplay between structure, proprioception, and autonomic regulation. This allows for a more targeted, brain-based approach that helps retrain the nervous system—without medication or invasive interventions.
You do not have to live on the edge of instability and exhaustion. With the right neurological inputs, your body can start to find its balance again—from the joints to the heart, and everything in between.
7. The Next Step: Find Out What Your Brain Is Trying to Tell You
If you have been struggling with hypermobility and symptoms of dysautonomia, we invite you to schedule a complimentary consultation with one of our doctors. Whether in person or over the phone, we will listen to your story, explain how our process works, and determine if chiropractic neurology is the right fit for you.
You have likely been searching for answers for a long time. Let us help you discover a brain-based path to stability.
If you or someone you love is suffering from a hypermobility syndrome and dysautonomia and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed References
- Celletti, C., Camerota, F., Castori, M., Censi, F., & Gioffrè, L. (2017). Evaluation of chronic fatigue and its correlations in patients with Ehlers-Danlos syndrome. Clinical and Experimental Rheumatology, 35(Suppl 107), 105-110.
- Raj, S. R. (2013). Postural tachycardia syndrome (POTS). Circulation, 127(23), 2336–2342. https://doi.org/10.1161/CIRCULATIONAHA.112.144501
- Rombaut, L., Malfait, F., De Paepe, A., Cools, A., Thijs, Y., & De Wandele, I. (2015). Impairment and impact of hypermobility type Ehlers–Danlos syndrome on daily life: a case–control study. American Journal of Medical Genetics Part A, 167(11), 2541–2550. https://doi.org/10.1002/ajmg.a.37268
- Mathias, C. J., Low, D. A., Iodice, V., Owens, A. P., & Kirbis, M. (2012). Postural tachycardia syndrome—Current experience and concepts. Nature Reviews Neurology, 8(1), 22–34. https://doi.org/10.1038/nrneurol.2011.187
