You walk into a brightly lit room, and suddenly your eyes squint, your head throbs, and your whole body feels tense. Maybe your heart rate spikes, your stomach turns, or you find yourself overwhelmed with irritation. If you have ever wondered why you react so strongly to lights—especially after a concussion, stress, or anxiety—you are not alone.

Many patients who struggle with light sensitivity feel dismissed. They are told it is all in their head. In truth, it is in the head—but not in the way they mean. It is neurological. And it is real.
In chiropractic neurology, we understand this phenomenon through the lens of brain function, particularly how the midbrain can become upregulated—overactive and overreactive—and what that does to your sensory system, emotions, and life.
This post is your guide to understanding what is happening in your brain and body when you experience light sensitivity, and what can be done to calm the chaos.
The Problem: Your Midbrain Is Stuck in Survival Mode
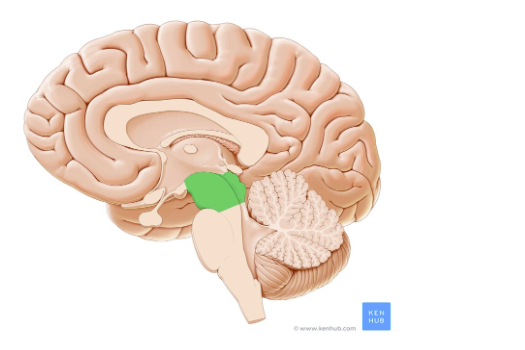 At the center of this story is a structure called the midbrain, or mesencephalon. It is part of your brainstem and sits between the upper brain (your cortex) and the lower brainstem (pons and medulla). The midbrain plays a major role in:
At the center of this story is a structure called the midbrain, or mesencephalon. It is part of your brainstem and sits between the upper brain (your cortex) and the lower brainstem (pons and medulla). The midbrain plays a major role in:
- Processing visual and auditory input
- Controlling eye movements and pupil constriction
- Initiating reflexive movements
- Coordinating basic emotional and defensive responses
When the midbrain is working normally, it filters and responds appropriately to incoming sensory information. But when it is upregulated—think of a volume knob turned too high—light, sound, and touch can become intolerable. A flickering light feels like a strobe. A passing siren feels like a punch. Wearing sunglasses everywhere you go – even inside – seems to be the only way to make it through the day.
This happens when the brain’s natural inhibitory pathways—mainly from the frontal lobe—fail to regulate the midbrain properly.
A Healthy Brain Is a Brain That Inhibits
This phrase is central to functional neurology. A healthy brain does not just react; it inhibits excessive reactions.
The frontal lobe, located at the front of the brain behind your forehead, is the command center for inhibition. It is responsible for:
- Executive functions (planning, focus, decision-making)
- Emotional regulation
- Motor control
- Filtering irrelevant stimuli
In a calm, well-functioning brain, the frontal lobe suppresses the lower brain centers (like the midbrain) from over-firing. This keeps your sensory experience balanced and your emotional responses proportional.
But when the frontal lobe is under-functioning—or when the midbrain is hyperactive due to trauma, stress, or inflammation—the brakes are off.
Suddenly, your brain cannot filter light correctly. It cannot tune down sound. And your tolerance for normal sensory input drops dramatically.
Common Triggers of Midbrain Dysregulation
Light sensitivity is not random. It often begins after a neurological stressor or injury. Common causes include:
1. Concussion and Traumatic Brain Injury (TBI) – LINK TO ARTICLE ABOUT CONCUSSION AND THE FRONTAL LOBE
Even a mild concussion can cause dysfunction in the frontal cortex and midbrain. Many people experience photophobia (light sensitivity), difficulty focusing, irritability, and heightened anxiety in the aftermath of a head injury.
The visual and auditory pathways run through the midbrain, and when inflammation or metabolic disruption hits that area, the sensitivity dial gets turned way up.
2. Chronic Stress
Chronic stress increases cortisol and sympathetic nervous system activity. This puts the brain into a state of hypervigilance, where midbrain circuits stay on high alert. Over time, the frontal lobe can become fatigued or underactive, making it harder to regulate sensory input and emotions.
3. Sensory Processing Disorders
In some individuals, particularly those with developmental challenges or neurodivergent traits (like autism spectrum disorder), the midbrain may not be inhibited properly from early life. This creates a lifelong pattern of sensitivity to light, sound, and touch.
4. Hormonal Fluctuations and Inflammation
Inflammation and hormone imbalances—especially those that affect neurotransmitter regulation—can lower inhibition and increase midbrain excitability. Migraine sufferers often report light sensitivity during hormonal shifts or times of systemic inflammation.
5. Dysautonomia and Autonomic Imbalance
Dysautonomia refers to a dysfunction of the autonomic nervous system (ANS), which controls involuntary functions like heart rate, blood pressure, digestion, and—critically—pupil response to light. Many people with dysautonomia experience symptoms like lightheadedness, heart palpitations, heat intolerance, and significant light sensitivity.
Why? Because the midbrain plays a role in autonomic regulation—especially in controlling pupillary reflexes and interacting with brainstem nuclei that manage sympathetic and parasympathetic tone. When autonomic function is disrupted, pupils may dilate excessively or fail to constrict appropriately in response to light, causing visual discomfort and overstimulation.
Additionally, in many types of dysautonomia (like POTS—Postural Orthostatic Tachycardia Syndrome), the body remains in a chronically heightened sympathetic state. This “fight-or-flight” mode keeps the midbrain overactive and contributes to a cascade of sensory overload and emotional instability.
For those with both dysautonomia and light sensitivity, midbrain regulation is a critical therapeutic target.
Midbrain, Light Sensitivity, and Emotional Outbursts: The Hidden Connection
It is not just about your eyes. The same midbrain structures that process light are also linked to emotional reactivity. When this area becomes overactive, your brain is not just over-responding to the environment—it is overreacting emotionally, too.
That means you might experience:
- Sudden bouts of anxiety
- Startle reflexes to sounds or sights
- Anger or crying episodes without clear cause
- Difficulty calming down after a stressor
This connection is rooted in how the midbrain interacts with the limbic system—especially the amygdala, which processes fear and threat. When your midbrain is overexcited, your amygdala tends to fire more easily, leading to emotional outbursts that feel impossible to control.
This can look like a child who screams at bright lights. Or an adult who panics in crowded stores. Or someone who seems to “snap” after a sensory trigger, then feels ashamed or confused afterward.
It is not weakness—it is neurology.
How Chiropractic Neurology Can Help
Chiropractic neurology approaches the brain as a dynamic, adaptable system. We do not just mask symptoms—we investigate why the brain is overreacting and work to restore balance.
We use targeted therapies to help:
1. Improve Frontal Lobe Activation
Through specific eye movement exercises, dual-task training, and cognitive stimulation, we can increase activity in the frontal cortex. This helps reinstate top-down inhibition of the midbrain.
2. Desensitize the Midbrain
We carefully reintroduce light, sound, and movement stimuli at a pace the brain can tolerate, using graded exposure. Over time, this teaches the midbrain to calm its responses.
3. Support Vestibular and Visual Integration
Midbrain dysfunction often co-occurs with balance or visual tracking issues. We assess and rehabilitate the vestibulo-ocular reflex (VOR), smooth pursuits, and saccadic eye movements—all of which tie into midbrain health.
4. Balance the Autonomic Nervous System
Techniques like respiration training, vagus nerve stimulation, and gentle sensory integration can help shift the nervous system out of fight-or-flight and into rest-and-digest.
What You Can Do at Home
While clinical care is key, you can also support your brain at home with these steps:
- Limit screen time and use blue light filters.
- Create sensory-friendly environments with natural lighting and low noise levels.
- Practice slow nasal breathing to activate the parasympathetic system.
- Use weighted blankets or deep pressure techniques to soothe an overactive brainstem.
- Prioritize sleep, hydration, and blood sugar regulation. A nourished brain inhibits better.
You Deserve a Brain That Feels Calm and in Control
Light sensitivity, anxiety, and emotional outbursts are more than inconveniences—they are signs your brain is struggling to regulate itself.
The good news? Neuroplasticity means your brain can change.
With the right support, you can train your brain to inhibit better, tolerate light and sound again, and regain control over your emotional responses. You are not broken. Your brain just needs a reset.
Want to Learn More? We Can Help
At Georgia Chiropractic Neurology Center, we specialize in functional brain-based care for people experiencing neurological dysregulation—from concussions to anxiety to sensory overload. We will assess your brain function and design a personalized plan to restore calm and clarity.
If you or someone you love is suffering from light sensitivity and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed Sources:
- Giza, C. C., & Hovda, D. A. (2014). The new neurometabolic cascade of concussion. Neurosurgery, 75(Suppl 4), S24–S33. https://doi.org/10.1227/NEU.0000000000000505
- Schindler, A., et al. (2021). Light sensitivity and visual dysfunction after traumatic brain injury: A review. Vision Research, 183, 1-9. https://doi.org/10.1016/j.visres.2021.01.002
- Rolls, E. T. (2015). Limbic systems for emotion and for memory, but no single limbic system. Cortex, 62, 119–157. https://doi.org/10.1016/j.cortex.2013.12.005
- Numan, M., & Woodside, B. (2010). Maternity, the limbic system, and midbrain pathways. Progress in Neurobiology, 90(3), 246–262. https://doi.org/10.1016/j.pneurobio.2009.10.007
- Thayer, J. F., Åhs, F., Fredrikson, M., Sollers, J. J., & Wager, T. D. (2012). A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neuroscience & Biobehavioral Reviews, 36(2), 747–756. https://doi.org/10.1016/j.neubiorev.2011.11.009
