You Have Found Solid Ground, But Your Brain Has Not
You step off a boat, a plane, or a treadmill. But instead of returning to the stability of dry land, it feels like you are still in motion. The floor rocks beneath you. The room gently sways. Days go by—and the sensation does not stop.
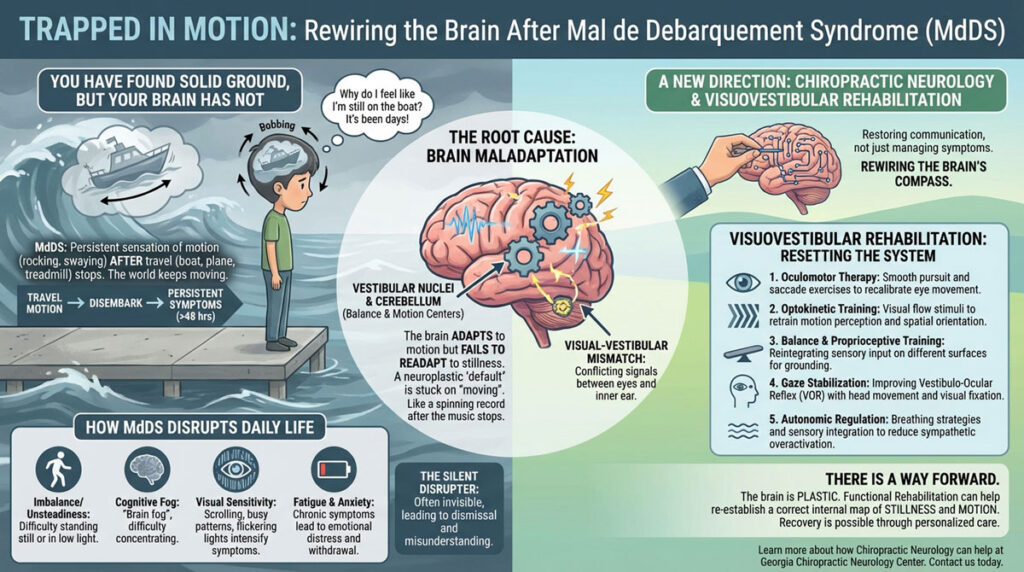
This is the frustrating and often misunderstood reality of Mal de Debarquement Syndrome (MdDS). For those living with this condition, the world never quite stops moving, even when everything around them is still. The disorientation, dizziness, and persistent internal rocking can derail work, relationships, and the simplest daily routines.
If you have felt unheard, misunderstood, or written off with this condition, you are not alone. Fortunately, recent developments in chiropractic neurology and visuovestibular rehabilitation are opening new doors for recovery.
Let’s walk through what MdDS is, how it affects daily life, why it occurs, and how chiropractic neurology can offer a new direction when the traditional approach has left you drifting.
What Is Mal de Debarquement Syndrome?
Mal de Debarquement Syndrome (MdDS) translates from French as “sickness of disembarkment.” It describes a persistent sensation of motion (rocking, swaying, or bobbing) that lasts well beyond the expected time after traveling—particularly after sea or air travel.
Unlike motion sickness, which occurs during movement, MdDS begins after the motion stops. In most cases, individuals notice symptoms within hours after disembarking from a cruise, flight, or even long car ride. For some, it can even be triggered by virtual reality or motion-based exercise equipment like treadmills.
While short-term disorientation is common after travel, MdDS becomes chronic when symptoms last for more than 48 hours. Some individuals experience spontaneous onset with no clear trigger, often complicating the diagnostic process.
How MdDS Disrupts Daily Life
MdDS can be a silent disrupter. Because there are typically no outward signs—no limp, no slurred speech—people with MdDS are often told they “look fine.” But their internal reality is anything but.
Common symptoms include:
- Persistent sensation of rocking, swaying, or bobbing (as if still on a boat)
- Imbalance or unsteadiness, especially while standing still or in low-light environments
- Cognitive fog or difficulty concentrating (“brain fog“)
- Sensitivity to visual motion or complex visual environments
- Fatigue
- Anxiety or depression related to chronic symptoms
These symptoms make daily tasks—grocery shopping, walking down a hallway, or driving—feel disorienting. Environments with busy patterns, flickering lights, or visual motion (like scrolling on a phone) can intensify symptoms.
Over time, quality of life often declines. Some individuals must leave their jobs, withdraw socially, or avoid places that trigger symptoms. Many also report being dismissed by clinicians unfamiliar with the condition, leading to emotional distress.
What Causes MdDS?
MdDS is still poorly understood in mainstream neurology, but emerging research points to maladaptation within the brain’s vestibular and sensory integration systems—especially how the brain processes and adjusts to motion and stillness.
The vestibular system, located in the inner ear and brainstem, helps detect head motion and orientation in space. When we are on a boat, our brain adapts to continuous motion through neuroplastic changes in the vestibular nuclei, cerebellum, and other sensory integration centers.
In MdDS, the brain fails to readapt once motion stops. Instead of returning to a still-state baseline, the central nervous system continues to perceive movement. Think of it like a record player that keeps spinning long after the music stops.
Some researchers also hypothesize that visual-vestibular mismatch—a misalignment between what the eyes see and what the vestibular system perceives—may perpetuate the syndrome.
This makes MdDS not just a vestibular condition, but a multisensory integration problem—a challenge chiropractic neurologists are uniquely trained to evaluate and treat.
Conventional Medical Treatment Options
Unfortunately, conventional medicine has few standardized protocols for MdDS. Many patients spend years consulting multiple providers before receiving a diagnosis.
Medical treatments typically include:
- Benzodiazepines (e.g., clonazepam): These may reduce motion perception temporarily, but are not curative and can be sedating or habit-forming.
- Selective serotonin reuptake inhibitors (SSRIs): Sometimes prescribed off-label to address comorbid anxiety or depression.
- Vestibular suppressants: Medications like meclizine or dimenhydrinate are usually ineffective, as they target peripheral rather than central vestibular mechanisms.
- Vestibular rehabilitation therapy (VRT): Traditional VRT can be helpful, but not always targeted toward MdDS-specific visuovestibular dysfunction.
- Repetitive Transcranial Magnetic Stimulation (rTMS): Experimental but promising results have been seen in altering abnormal brain activity in select areas like the entorhinal cortex or prefrontal regions.
Many individuals are told there is no known cure, leaving them to manage symptoms indefinitely. However, a chiropractic neurology approach reframes the condition not as permanent damage, but as a functional mismatch—one that can be recalibrated.
A Chiropractic Neurology Approach to MdDS
At its core, chiropractic neurology focuses on restoring proper communication between the brain and body through functional rehabilitation—without pharmaceuticals or surgery.
Because MdDS involves dysfunction in how the brain integrates motion, space, and sensory input, the chiropractic neurology model is well-suited to assess and rehabilitate the systems involved.
One of the most powerful tools in this process is visuovestibular rehabilitation.
Visuovestibular Rehabilitation—Resetting the Brain’s Compass
Visuovestibular rehabilitation involves exercises that recalibrate how the brain interprets visual and vestibular input. It is not simply balance training, but a carefully designed series of stimulus-response exercises that engage multiple areas of the brain, including:
- Vestibular nuclei in the brainstem
- Cerebellum, which helps coordinate motion and balance
- Parietal lobe, which integrates body position and spatial awareness
- Frontal lobe, which inhibits inappropriate sensory responses and directs attention
- Oculomotor centers involved in eye movement and gaze stability
In MdDS, these systems have learned an incorrect sensory “default.” Visuovestibular therapy teaches the brain to unlearn the false motion and return to accurate spatial grounding.
A typical chiropractic neurology approach might include:
1. Oculomotor Therapy
Smooth pursuit, saccade, and fixation exercises help recalibrate eye movement and reduce visual-vestibular mismatch.
2. Optokinetic and Visual Flow Training
These are moving visual stimuli (such as stripes or scrolling dots) used to retrain the brain’s motion perception systems and recalibrate spatial orientation.
3. Balance and Proprioceptive Training
Working on different surfaces or head positions helps reintegrate vestibular and somatosensory input to improve grounding and spatial certainty.
4. Gaze Stabilization Exercises
Combining head movement with visual fixation improves vestibulo-ocular reflex (VOR) function, which is often disrupted in MdDS.
5. Autonomic Nervous System Regulation
Chiropractic neurologists may assess dysautonomia (common in MdDS) and incorporate breathing strategies, eye movement exercises, or light/sound integration to downregulate sympathetic overactivation.
Why This Approach Works
The brain is plastic. While MdDS is disorienting and persistent, it is not a fixed structural problem—it is a functional mismatch. By giving the brain targeted sensory input, we can help it re-establish a correct internal map of stillness and motion.
Recovery is often non-linear, but many individuals experience noticeable improvements in grounding, clarity, and symptom relief with a personalized, progressive program. The key is individualization: no two MdDS cases are exactly alike.
There Is a Way Forward
If you are living with MdDS, you may feel like your feet never fully touch the ground. But you are not stuck. You are not broken. Your brain simply needs the right tools to reorient.
At Georgia Chiropractic Neurology Center, we believe that conditions like MdDS require more than symptom management—they require a strategic rewiring of the brain’s sensory systems. Through detailed assessment and customized visuovestibular rehabilitation, we help patients step back into stable, grounded lives.
If you or someone you love is suffering from Mal de Debarquement syndrome and you would like to learn how chiropractic neurology can help, contact the team at Georgia Chiropractic Neurology Center today. We look forward to hearing from you.
Written by Sophie Hose, DC, MS, DACNB, CCSP
Peer-Reviewed References
- Cha Y-H. (2015). Mal de debarquement. Seminars in Neurology, 35(5), 587–594. https://doi.org/10.1055/s-0035-1563575
- Yakushin SB, Minor LB, Raphan T, Cohen B. (2017). Orientation of the internal representation of head direction in patients with MdDS. Journal of Neurophysiology, 118(5), 2801–2812. https://doi.org/10.1152/jn.00456.2017
- Cohen H, et al. (2018). Vestibular rehabilitation in MdDS: Effectiveness of optokinetic stimulation. Frontiers in Neurology, 9, 887. https://doi.org/10.3389/fneur.2018.00887
- Hain TC, Hanna PA, Rheinberger MA. (1999). Mal de debarquement. Archives of Otolaryngology–Head & Neck Surgery, 125(6), 615–620. https://doi.org/10.1001/archotol.125.6.615
